PSSM1 / PSSM2 / MIM / MFM / RER – when sugar becomes a health hazard
What causes PSSM, MIM MFM and RER, and how are they diagnosed?
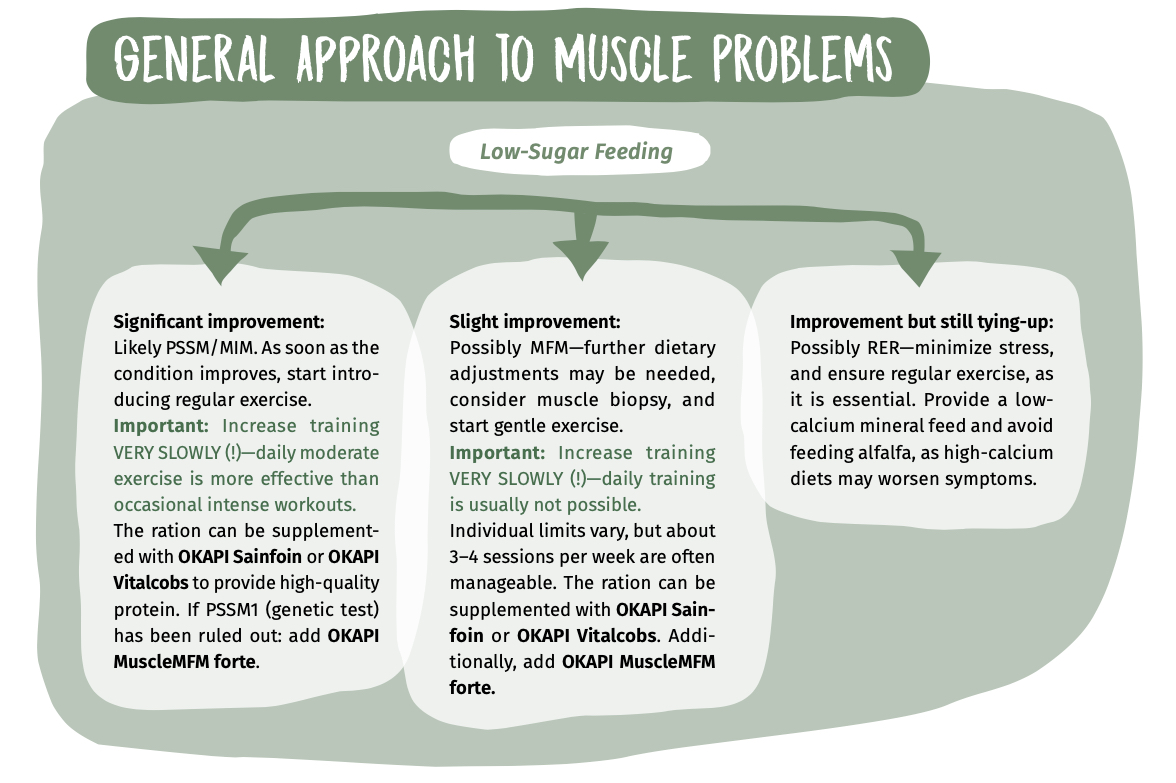
All of these conditions are muscle metabolism disorders that can only be accurately diagnosed through muscle biopsy.
The MIM genetic test is scientifically controversial because the deficient enzyme has not yet been clearly associated with PSSM2, MFM, or RER. Additionally, the test lumps together different types of myosillites that have distinct causes and require different management approaches. While PSSM2 responds primarily to training and low-sugar feeding, MFM affects the myofibril structure and requires targeted nutrition, feed support, B6 involves polysaccharide carbohydrate regulation and requires a low-starch diet. MIM is not a scientifically recognised diagnosis. Reliable diagnosis should always be based on clinical symptoms, muscle biopsy findings, and individually tailored management and nutrition plans.
PSSM 1:
Which horse breeds are primarily affected by PSSM1?
Certain breeds—including Appaloosa, Paint Horse, Quarter Horse, and various draft horse breeds, as well as their crosses—are affected by an autosomal dominant hereditary disorder known as PSSM1. This condition involves abnormal glycogen storage in the muscles.
Muscle sugar storage damages tissue
Affected horses show glycogen levels in their muscles that are two to four times higher than healthy horses. This excessive storage can cause muscle damage. In Quarter Horses and Appaloosas, symptoms typically appear by young age and while draft horses tend to experience generally weakening and muscle wasting.
Young horses can be affected too
Foals and young horses can develop type-up symptoms under certain stress conditions, such as respiratory or gastrointestinal illness. Abnormal glycogen storage typically begins around 16 months of age and primarily affects type II muscle fibers. Horses that also carry a malignant hyperthermia (MH) mutation tend to respond poorly to low-sugar diets and regular training.
Treatment and prevention
A combination of targeted feeding and structured training can lead to a noticeable reduction in creatine kinase (CK) levels within just three weeks. Without consistent exercise, CK levels can rise above 1000U/L. A gradual training approach is essential—start with just a few minutes of walking and trotting, increasing the duration by one to two minutes daily. However, too rapid an increase in workload can backfire—even ten minutes of walking may trigger a tying-up episode.
Diagnosis
Diagnosis relies on a genetic test for the GYS1 mutation and significantly elevated CK levels in the blood. A muscle biopsy may also confirm symptoms are caused by PSSM1.
Feeding plays a key role
Low-sugar hay with a sugar content below 6%, combined with balanced mineral supplementation, is essential but only effective when paired with regular exercise. If the hay’s sugar content is too high, it should be soaked before feeding. Chromium-containing supplements should be avoided, as they enhance glucose uptake into muscle cells. L-carnitine should also be used with caution, as it can increase glucose uptake and may worsen disease progression.
PSSM 2 / MIM:
Symptoms often appear later in life
PSSM2 is an umbrella term for several myopathies that differ from PSSM1 in that they are not caused by a GYS1 mutation. Unlike PSSM1, PSSM2 can potentially affect all horse breeds, though Warmbloods appear particularly susceptible. Among Warmbloods, dressage horses are affected more frequently than jumpers. Initial clinical signs typically appear around six years of age or older.
PSSM2 shows up more in movement patterns
Tying-up episodes are much less common in PSSM2. Instead, it often presents as stiffness, shortened stride, lack of forward movement, and mild hindlimb lameness with no clearly identifiable cause. Gait abnormalities and ridability issues are the most common initial symptoms in Warmbloods, occurring in about 66% of affected horses.
Diagnosis is challenging
Among Warmbloods, older horses and geldings are more frequently affected than in other breeds. However, unlike PSSM1, no specific genetic test has been identified as particularly susceptible to the condition. Muscle analysis shows that glycogen concentrations in Warmbloods with PSSM2 are similar to those in healthy horses. In contrast, Quarter horses with PSSM2 tend to have elevated muscle enzyme levels, CK (creatine kinase) and AST (aspartate aminotransferase) enzyme levels in PSSM2 often fall within the normal range.
Diagnosis through dietary management
Clinical symptoms can improve through a targeted combination of diet and exercise. However, even minor changes in feeding management can cause setbacks. If the recommended PSSM2 diet doesn’t yield results, switching to the feeding strategy used for MFM (Myofibrillar Myopathy) may help. There is evidence suggesting that PSSM2 may represent an early stage of MFM.
Feeding recommendations for PSSM2
Feeding should focus on low-sugar hay with a sugar content below 6%, combined with a high-quality mineral supplement. To support muscle development, saffloin can be added to the diet. At the same time, exercise must be carefully managed—a slow and steady training program is essential to avoid over-exertion and stabilize muscle metabolism.
NOTE:
MIM is a label introduced to justify the associated genetic tests. It is not a separate medical condition. Affected horses fall within the PSSM2 spectrum.
MFM:
Usually affects Arabians and Warmbloods
MFM (Myofibrillar Myopathy) primarily affects Arabians and Warmbloods, with most affected horses being older (8-10 years).
Tying-up episodes or PSSM2-like symptoms
In Arabians, MFM can cause muscle stiffness and occasional tying-up episodes. In Warmbloods, clinical signs tend to resemble those of PSSM2. CK and AST levels in Warmbloods with MFM usually remain within normal ranges, while in Arabians they may be slightly elevated—but not to the extent typically seen with classic tying up.
Diagnosis via muscle biopsy
A hallmark of MFM is the presence of desmin aggregates and excess glycogen in muscle fibers, both of which can be detected through muscle biopsy.
No mutation, but reduced muscle regeneration
A desmin gene mutation does not appear to be the cause of MFM in Arabians. The glycogen accumulation may instead be linked to degenerated myofilaments and remnants of the Z-discs. Additionally, there is reduced expression of genes involved in muscle regeneration.
Increased fatty acid transport and impaired cysteine biosynthesis
MFM horses show an enhanced ability to transport fatty acids into mitochondria. However, this leads to higher production of reactive oxygen species (ROS), while the body’s ability to neutralize them is reduced. The antioxidant PRDX6 is expressed at four times lower levels in MFM horses. Impaired cysteine biosynthesis may also play a role, as a cysteine deficiency limits the ability of glutathione to buffer irreversible oxidation.
Feeding and management
The diet should consist of low-sugar hay (<6%) and inorganic mineral feed. To support muscle development, the ration can be supplemented with saffloin or alfalfa. Targeted amino acid supplementation is also beneficial—especially lysine, methionine, and threonine. Additional supplements may include cysteine (important for antioxidants), valine, leucine, and isoleucine (to support post-exercise protein synthesis), as well as sulfur. Horses without pasture access also benefit from added vitamin E.
Training is important—but must be tailored
Gradual progression in training is essential. Exercise tolerance in MFM horses is highly individual, but moderate sessions 3-4 times per week are usually well tolerated.
RER:
Primarily affects Thoroughbreds, Standardbreds, and Arabians
Recurrent Exertional Rhabdomyolysis (RER) is a hereditary muscle disorder in horses caused by disrupted calcium regulation within muscle cells. This leads to repeated episodes of muscle cramping and stiffness, especially during or after exercise. RER occurs most frequently in Thoroughbreds, Standardbreds, and Arabians.
No mutation identified so far
There is a genetic predisposition, but no specific mutation has been identified to date. Horses with nervous temperaments or high stress levels are more likely to develop RER.
Symptoms
The main signs of RER include muscle stiffness and cramping during or after physical exertion. Affected horses often show restlessness, excessive sweating, and reluctance to move. In severe cases, urine may appear dark, indicating myoglobinuria caused by muscle tissue breakdown. Muscle tremors or spasms may also be present.
Multiple triggers
Stress and excitement increase muscle tension, while unfamiliar or excessive physical strain can trigger RER episodes. Faulty calcium regulation in the muscle leads to excessive contractions, which intensify the symptoms. Diets high in starch and sugar can also increase the risk by heightening nervous system excitability.
Diagnosis
Diagnosis is based on clinical evaluation during or shortly after an episode, as well as blood tests showing elevated muscle enzymes such as creatine kinase (CK) and aspartate aminotransferase (AST). In some cases, a muscle biopsy may be performed to confirm the diagnosis.
Management and feeding
A diet low in starch and sugar helps stabilize energy supply and reduce excitability. Regular exercise is essential to prevent muscle tension. A low-stress environment and carefully structured training routine can help minimize episode frequency. In some cases, medication such as dantrolene or other trolyte supplements may be used to regulate muscle tension and improve the horse’s overall well-being.
- Fundamentals of Equine Anatomy: The Musculoskeletal System - 13. January 2026
- How Does a Horse Move? Biomechanics of the Basic Gaits - 13. January 2026
- The Horse’s Carrying System – Why the Equine Back Needs Training - 13. January 2026










